Abstract
Introduction:
Central nervous system (CNS) relapse in diffuse large B-cell lymphoma (DLBCL) is rare and associated with poor outcome. The presence of MYC rearrangement (MYC -R)with or without BCL2 and/or BCL6 rearrangement (high-grade B-cell lymphomas, or HGBCL, per 2016 WHO revision) has been associated with inferior survival with traditional R-CHOP chemotherapy and a higher incidence of CNS relapse. The incidence of CNS relapse and patient outcome in patients with HGBCL and MYC -R with increasing use of aggressive CNS directed chemotherapy or CNS prophylaxis is unknown.
Methods:
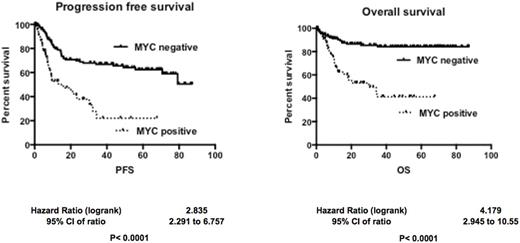
In this single-center retrospective cohort study we compared the incidence of CNS relapse in HGBCL with at least MYC -R (MYC- R group) with DLBCL not otherwise specified (DLBCL NOS, non- MYC -R group). Differences between groups were analyzed using Chi-square, Fisher's exact and t-Student tests. Statistical significance was set at P<0.05. Kaplan Meier method was used to calculate progression-free survival (PFS) and overall survival (OS). Log-rank test was used to determine differences in survival. Statistical analyses were performed using SPSS.24 software.
Results:
Of 205 patients, 72 (35%) were MYC -R and 133 (65%) were non- MYC -RDLBCL. The median age at diagnosis was 62 (range 18-70 years), and 126 patients were male (61%). The MYC -R (HGBCL) group included 58 (80%) patients with concurrent BCL2 and/or BCL6 rearrangement. Among MYC -R patients, 42 (58%) had a high-intermediate or high international prognostic score (IPI) score, 61 (of 68; 90%) were of germinal center B-cell (GCB) type, and 56 (of 69; 81%) presented with advanced stage disease. Among non- MYC -R patients, 49 (of 121; 40%) had high-intermediate or high IPI, and 90 (of 132; 68%) had advanced stage disease. For treatment, 28 (of 66; 42%) MYC -R and 31 (of 120; 25%) non- MYC -R patients received CNS prophylaxis either as intrathecal methotrexate or cytarabine or as systemic therapy with high-dose methotrexate. One MYC -R patient had CNS involvement at presentation. Chemotherapy among MYC -R patients included R-CHOP (23 patients), R-HyperCVAD (8), DA-R-EPOCH (27), R-CHOEP (4) and other diverse regimens including clinical trials (6). Among non- MYC -R patients, regimens included R-CHOP (102), R-HyperCVAD (3), DA-REPOCH (9), and R-CHOEP (13). CNS relapse was seen in 4 patients in the MYC -R group (5.6%) and 1 patient (0.7%) in the non- MYC -R group (P=0.053). Three of the 4 MYC -R patients with CNS relapse had received CNS prophylaxis. The non- MYC -R patient who had CNS relapse initially presented with CNS involvement and had been treated with high dose methotrexate. Twenty-six (26) MYC -R patients and 24 non- MYC -Rpatients had primary refractory disease. Median PFS was 15.9 months in MYC- R vs. not reached in non- MYC- R (HR 2.835; 95% CI 2.291 to 6.757, P<0.0001), and median OS was 30 months in MYC- R vs. not reached in non- MYC- R (HR 4.179; 95% CI 2.945 to 10.55, P<0.0001).
Conclusion:
The incidence of CNS relapse among both MYC -R (HGBCL) and non- MYC -R (DLBCL NOS) cohorts was overall low and may have been mitigated with the use of prophylaxis. Although, CNS relapse occurred despite CNS prophylaxis in both groups. Both the PFS and OS among MYC -R patients were significantly worse compared to non- MYC -R patients despite the use of more aggressive therapy in a majority of MYC- R patients. Larger studies are needed to confirm these findings and determine optimal strategies for CNS prophylaxis and therapy in HGBCL and DLBCL NOS.
Reddy: BMS: Consultancy; Celgene: Consultancy; Abbvie: Consultancy; Gilead: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal